Where healing
begins
We specialize in restoring hope


Why Coflex®?

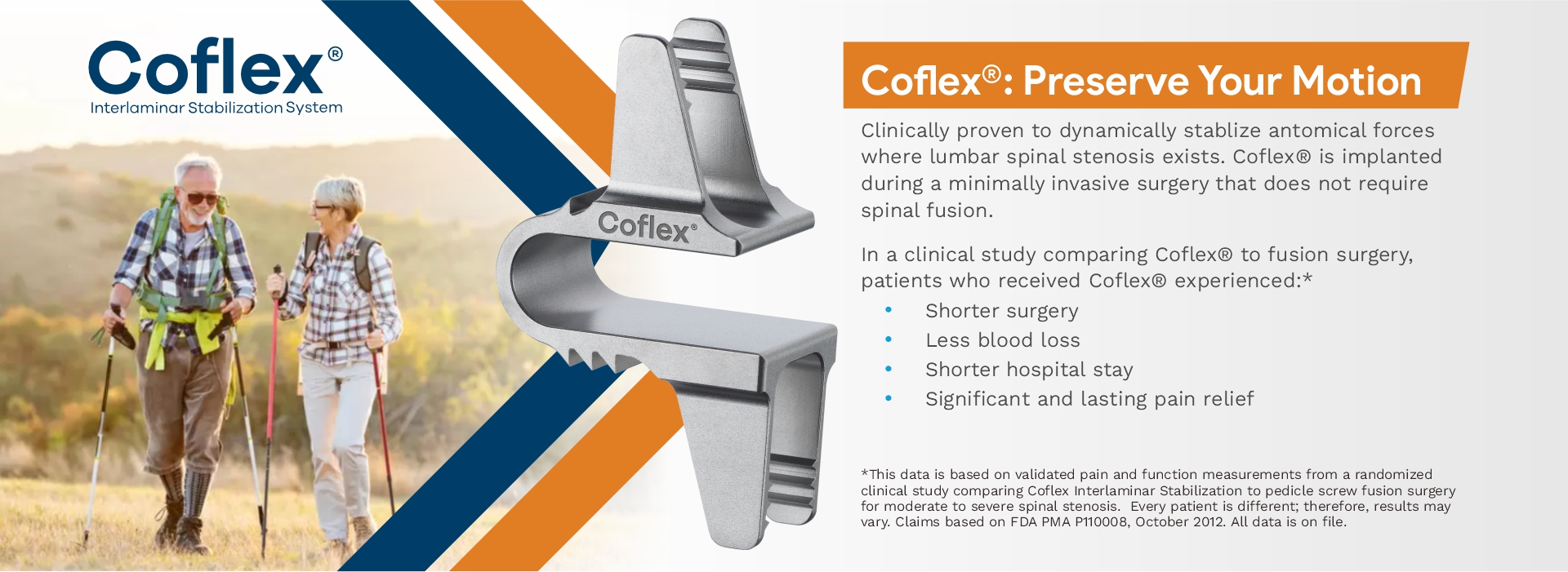
If non-surgical treatment options aren’t successful, it may be time to consider surgery. Decompression with Coflex® Interlaminar Stabilization is an alternative to fusion, that reduces pain, and helps preserve mobility.
Coflex® is the only posterior lumbar motion preservation solution with proven long-term outcomes for durable pain relief and stability. The “U” shape design allows Coflex® to be positioned on the strongest bony structure of the posterior column, the lamina. Coflex® maintains the height between the bones in your spine to help the nerves move freely.
Coflex® is an option for patients that do not want to go through pedicle screw fusion, but for whom a decompression alone would not offer needed stability.
Why Coflex®?

If non-surgical treatment options aren’t successful, it may be time to consider surgery. Decompression with Coflex® Interlaminar Stabilization is an alternative to fusion, that reduces pain, and helps preserve mobility.
Coflex® is the only posterior lumbar motion preservation solution with proven long-term outcomes for durable pain relief and stability. The “U” shape design allows Coflex® to be positioned on the strongest bony structure of the posterior column, the lamina. Coflex® maintains the height between the bones in your spine to help the nerves move freely.
Coflex® is an option for patients that do not want to go through pedicle screw fusion, but for whom a decompression alone would not offer needed stability.

For decades, the surgical options for patients with lumbar spinal stenosis (LSS) were limited to either decompression or decompression with spinal fusion. In 2012, the FDA approved Coflex®, a small U-shaped titanium implant that provides spinal stability without the invasiveness and loss of mobility associated with spinal fusion.
For decades, the surgical options for patients with lumbar spinal stenosis (LSS) were limited to either decompression or decompression with spinal fusion. In 2012, the FDA approved Coflex®, a small U-shaped titanium implant that provides spinal stability without the invasiveness and loss of mobility associated with spinal fusion.
Our Patients Share Their Coflex® Success Stories

To learn more about Ken’s experience, watch this
video:
“After my surgery I thought it was going to be a long process of recovery, within about 3 days I was up and walking around, within a week or so I was walking around the block a couple of times, within about 3 weeks I was able to walk without any problem whatsoever.”
-Ken-
Our Patients Share Their Coflex® Success Stories

To learn more about Ken’s experience, watch this
video:
“After my surgery I thought it was going to be a long process of recovery, within about 3 days I was up and walking around, within a week or so I was walking around the block a couple of times, within about 3 weeks I was able to walk without any problem whatsoever.”
-Ken-
Click Here To Watch More Patient Success Story Videos
Click Here To Watch More Patient Success Story Videos
In the FDA study, 94% of patients were satisfied
with their outcomes after two years.*
Ask your doctor if you’re a candidate
for Coflex®.

“Coflex® has become a device that can change people’s lives. It changes the length of stay for surgery, the recovery, the ability to return to activities that they weren’t able to do before in a shorter period of time.”
Andrew Fox
In the FDA study, 94% of patients were satisfied
with their outcomes after two years.*
Ask your doctor if you’re a candidate
for the Coflex®.

“Coflex® has become a device that can change people’s lives. It changes the length of stay for surgery, the recovery, the ability to return to activities that they weren’t able to do before in a shorter period of time.”
Andrew Fox
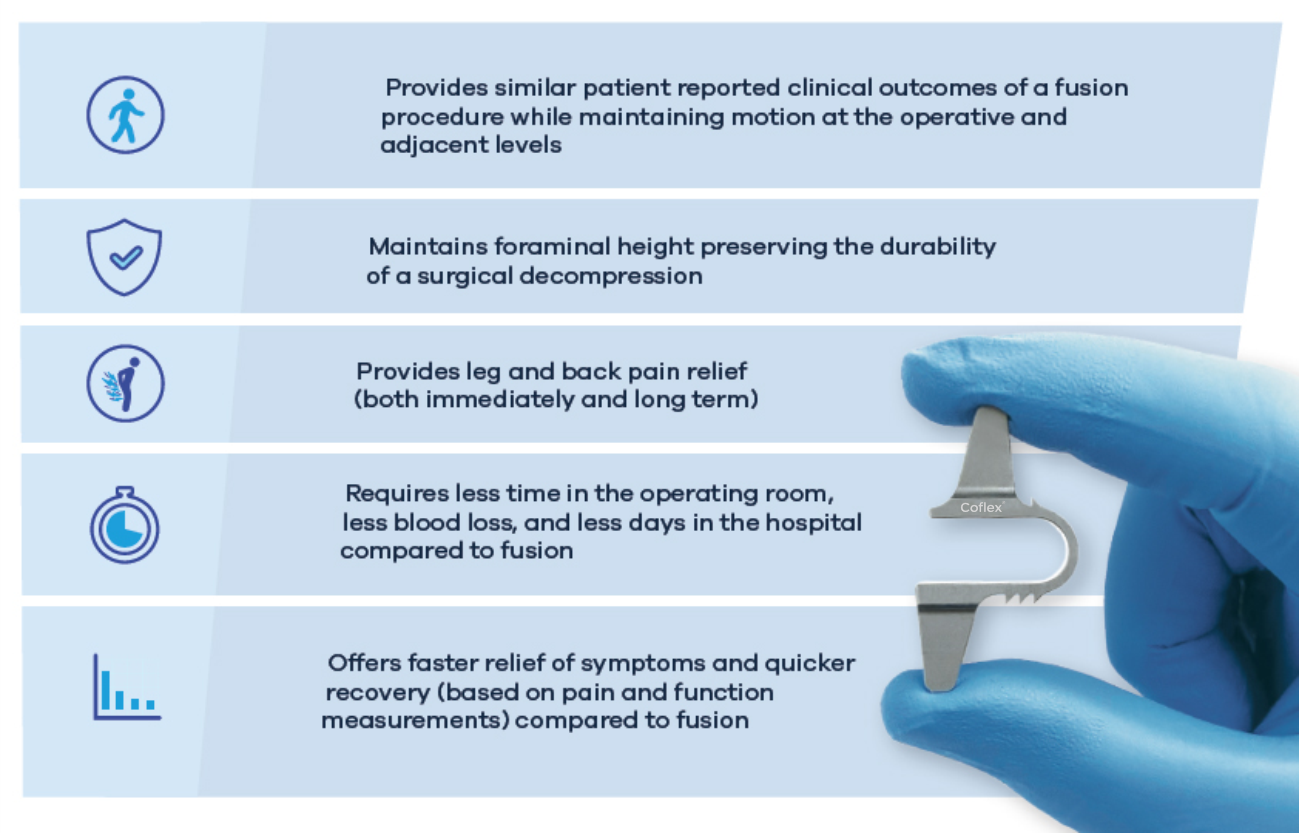
Benefits of Coflex® vs. Fusion’
Pedicle screws and rods are used to fuse bones together – a highly-invasive spinal stenosis surgery that can sometimes result in loss of motion and a long and arduous recovery process. In a U.S. FDA study, Coflex® proved to be a beneficial alternative to pedicle screw fusion. The results showed that patients with Coflex® performed as well, if not better, in all clinical measurements The patients who received Coflex® experienced:

- Leg and back pain relief (both
immediately and long-term) - Less time in the operating room, less blood loss, and fewer days in the hospital
- Faster relief of symptoms and
quicker recovery (pain and function measurements) - Maintenance of range of motion at both treated and adjacent segments
This data is based on validated pain and function measurements from a randomized clinical study comparing Coflex Interlaminar Stabilization to pedicle screw fusion surgery for moderate to severe spinal stenosis. Every patient is different; therefore, results may vary. Claims based on FDA PMA P110008, October 2012. All data is on file

What to Expect for Your Procedure
Setting expectations for your surgery ahead of time will give you peace of mind when the day of the procedure arrives. Be sure to give yourself and/or caregiver time to prepare and create a plan for after the surgery occurs.
What to Expect for Your Procedure
Setting expectations for your surgery ahead of time will give you peace of mind when the day of the procedure arrives. Be sure to give yourself and/or caregiver time to prepare and create a plan for after the surgery occurs.
Preparing for Surgery
In order to feel prepared and confident as your procedure approaches, it may be helpful to learn a little bit more about what will happen during your surgery. Coflex procedures can be performed in an outpatient setting. You should arrange for someone to drive you, and to help during the first few hours of your recovery after surgery.
Before surgery, you might also want to ask your spine surgeon for more information such as:
- When can I expect to be back home from surgery?
- Is there anything else that I should do to prepare in the days leading up to surgery?
- What can my caregiver do to help me prepare?

Preparing for Surgery
In order to feel prepared and confident as your procedure approaches, it may be helpful to learn a little bit more about what will happen during your surgery. Coflex procedures can be performed in an outpatient setting. You should arrange for someone to drive you, and to help during the first few hours of your recovery after surgery.
Before surgery, you might also want to ask your spine surgeon for more information such as:
- When can I expect to be back home from surgery?
- Is there anything else that I should do to prepare in the days leading up to surgery?
- What can my caregiver do to help me prepare?

The Surgical Procedure
Decompression surgery involves removing the pressure on the nerves that causes pain. After undergoing decompression surgery, Coflex® will be inserted through the incision made for the decompression. Coflex® is positioned on your lamina, which is the strongest bone in the back of your spine. On average, the entire procedure, including decompression and the implantation of Coflex®, takes approximately 100 minutes.

Recovery
Most patients are under general anesthesia, so a short recovery period is necessary following the procedure.
Immediately following surgery
When you wake from recovery, you may be encouraged to get up and walk almost immediately, taking into consideration your overall health at the time of surgery. Since there is no fusion, and therefore no healing bone to wait for, you’ll most likely be able to do this right after your procedure. You’ll notice that your pain has been significantly relieved, and your spine should feel stable and strong. Most patients do need to wait several days following the surgery for the incision wound to heal.’
Weeks and months following surgery
In the weeks and months following surgery, your recovery depends on a number of factors, including the degree of your stenosis and the extent of the decompression that was performed. Most patients are able to return to normal activity, and even expanded activity such as golf, cycling, or gardening, within weeks of the surgery. Some patients may require physical therapy to help with mobility and flexibility.’
The Surgical Procedure
Decompression surgery involves removing the pressure on the nerves that causes pain. After undergoing decompression surgery, Coflex will be inserted through the incision made for the decompression. The Coflex device is positioned on your lamina, which is the strongest bone in the back of your spine. On average, the entire procedure, including decompression and the implantation of Coflex, takes approximately 100 minutes.


Recovery
Most patients are under general anesthesia, so a short recovery period is necessary following the procedure.
Immediately following surgery
When you wake from recovery, you may be encouraged to get up and walk almost immediately, taking into consideration your overall health at the time of surgery. Since there is no fusion, and therefore no healing bone to wait for, you’ll most likely be able to do this right after your procedure. You’ll notice that your pain has been significantly relieved, and your spine should feel stable and strong. Most patients do need to wait several days following the surgery for the incision wound to heal.’
Weeks and months following surgery
In the weeks and months following surgery, your recovery depends on a number of factors, including the degree of your stenosis and the extent of the decompression that was performed. Most patients are able to return to normal activity, and even expanded activity such as golf, cycling, or gardening, within weeks of the surgery. Some patients may require physical therapy to help with mobility and flexibility.’
Coflex® is the FIRST AND ONLY posterior lumbar motion preservation solution with Level I evidence (the highest possible level of clinical data) from two prospective randomized studies against two treatment options.’ There are many peer-reviewed publications on Coflex®, making it one of the most studied lumbar spinal devices on the market. Coflex® has been implanted in more than 175,000 patients in over 60 countries.
This makes Coflex® the only posterior lumbar motion preservation solution with proven long-term outcomes for durable pain relief and stability.
Coflex® is the FIRST AND ONLY posterior lumbar motion preservation solution with Level I evidence (the highest possible level of clinical data) from two prospective randomized studies against two treatment options.’ There are many peer-reviewed publications on Coflex®, making it one of the most studied lumbar spinal devices on the market. Coflex® has been implanted in more than 175,000 patients in over 60 countries.
This makes Coflex® the only posterior lumbar motion preservation solution with proven long-term outcomes for durable pain relief and stability.
90% Coflex® vs 77% spinal fusion?
- At six weeks, Coflex® patients experienced Quicker relier of their symptoms when compared to spinal fusion patients
94% Coflex@ vs 87% spinal fusion?
- At two years, Coflex® patients had longer
lasting relief of their symptoms compared to spinal fusion.
94% Coflex® vs 87% spinal fusion?
- At five years, Coflex® patients were happier with their outcomes when compared to patients that underwent spinal fusion
To ensure that you have all the information you or your loved ones need, below are the questions most asked by patients who’ve used Coflex®: